Insulation Energy Appraisal in Health-Care Facilities: A Case Study
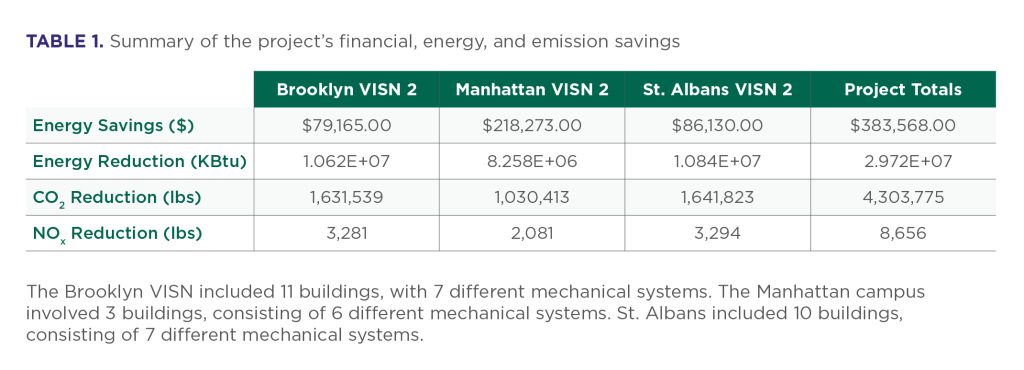
When RWE Clean Energy, headquartered in Austin, Texas, partnered with Irex Energy Solutions (Irex), an NIA member company based in Quarryville, Pennsylvania, to assess three Veterans Administration (VA) hospital campuses, the project demonstrated how systematic insulation energy appraisals can deliver exceptional return on investment (ROI) in health-care environments. This appraisal case study encompassed more than 10 buildings across 3 Veterans Integrated Service Networks (VISN) hospital and assisted-care living facilities in Brooklyn, Manhattan, and St. Albans, New York. Total energy cost savings across all facilities exceeded $380,000.00, and emissions were reduced by more than 4.3 million pounds of CO2.
The project’s success stemmed from an appraisal process that addressed the unique operational challenges of health-care facilities while maintaining thorough technical standards. The implementation delivered energy savings that exceeded the original projections, generating sufficient cost savings to fund additional energy conservation projects across the health-care system. Table 1 shows the dollar, energy, and emission reduction data for each of the campuses as well as project totals.
RWE Senior Director of Programs and Implementation Andre Le Blanc noted that the VA’s ROI required payback period is longer than many facilities, at 7 years, adding, “As an ECM [energy conservation measure], we call insulation ‘low-hanging fruit.’ If I go into a facility and I see that they’ve got insulation issues, generally it has a really compelling ROI related to the insulation improvements. Right off the bat, we know it is going to meet budget constraints.”
Project Background and Methodologies
The VA health-care system operates some of the most energy-intensive facilities in the federal portfolio, requiring continuous operation, precise environmental controls, and robust steam systems for humidity management critical to patient care. The three campuses included in this case study’s assessment exemplified common challenges within the VA health-care infrastructure, including the fact that the core buildings were constructed in the 1940s and have undergone decades of modifications and repair—often without corresponding attention to insulation maintenance, which is viewed as an expense rather than an investment.
The assessment methodology combined systematic technical evaluation with specialized protocols required for health-care facility access. The project team structured their approach in two distinct phases, designed to maximize data collection while minimizing disruption to hospital operations.
Phase 1: Comprehensive On-Site Evaluation
The 2-week on-site evaluation employed a two-person appraisal team with an off-site dedicated note-taker, working within the constraints of health-care facility protocols. Every mechanical room required escort personnel, which was a security requirement.
The technical evaluation focused on detailed mechanical room takeoffs involving precise measurements of bare pipes, fittings, and valves. The appraisal team employed three critical assessment techniques, including:
- Systematic visual inspection: Complete documentation of all insulation conditions, with particular attention paid to missing insulation and severely damaged sections. The approach was intentionally comprehensive, documenting all issues, regardless of immediate payback potential, to provide complete data for informed client decision making.
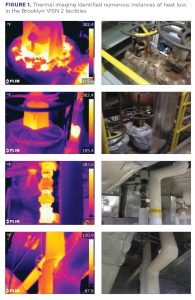
- Infrared thermal imaging: Heat signature analysis to identify energy loss areas not apparent through visual inspection alone. This technology proved particularly valuable for identifying steam system inefficiencies, which represented the greatest energy loss opportunities across all facilities.
- Precision measurement: Pipe diameter assessment using calipers and tape measures to ensure accurate calculations for insulation requirements and energy savings projections.
According to NIA Certified Insulation Energy Appraiser Andrew Martin of Irex, the reports generated from the appraisal are where the shock-and-awe factor come in, noting, “You may feel the heat when you walk in a room, and look around and might not see much missing insulation, but the thermal imaging shows how all the small uninsulated areas add up.”
Phase 2: Analysis and Engineering Calculations
The 2-week off-site analysis phase transformed field data into actionable recommendations, using 3E Plus® software to calculate energy savings based on process temperatures and ambient conditions. RWE provided the following criteria for the calculations: process temperatures, hours of operation for each system, ambient air temperature of the mechanical areas, fuel type/cost, and efficiency of the system(s).
A critical aspect involved reconciling energy code requirements and VA construction standards with existing building constraints. “Actual installation may not meet code requirements, due to space constraints in existing buildings,” Martin noted. This reality required engineering solutions that balanced optimal energy performance with practical installation considerations.
The analysis phase also incorporated customer-provided operational data, including boiler efficiency and system operational requirements, ensuring that calculations reflected actual facility conditions, rather than theoretical scenarios.
Hospitals maintain large steam loads, primarily for the humidity control essential for patient comfort, surgical suite performance, and infectious disease control. This operational reality means insulation improvements around steam systems deliver benefits beyond energy savings, contributing directly to clinical care quality. The assessment revealed that steam systems showed the greatest energy losses across all facilities, making these improvements both high impact from an energy perspective and operationally critical for health-care standards.
Thermal imaging analysis revealed energy dissipation patterns extending beyond visually obvious problems, identifying heat loss through damaged insulation that appeared intact during casual inspection. This comprehensive documentation approach proved strategically valuable—while some areas showed marginal individual returns, the complete scope enabled informed decisions about phasing improvements to maximize overall impact. See Figure 1 through Figure 3 for before and after images from each of the three campuses.

Implementation Process: From Appraisal to Operational Results
The appraisal findings were presented as part of a package for review and decision-making by the federal government for the VA system based on anticipated ROI. According to Le Blanc, “For insulation, you can see it—you can see what has been removed. You can feel it. You can feel the heat coming off the areas of piping. You can do infrared testing and see where the energy is being let out. The insulation work is often more straightforward than other ECMs.”
Once the appraisal results were presented to VA decision-makers, the transition from assessment to implementation required careful planning to address the challenges of health-care facility construction while maintaining operational continuity.
Implementation Strategy
The complete implementation required 18 to 22 months, with the extended timeline reflecting comprehensive improvement scope and specialized health-care facility requirements. The process followed a carefully sequenced approach.
- Custom blanket fabrication: Initial site work included measuring and specifying removable insulation blankets, followed by several months of off-site fabrication. This approach enabled custom-fitted solutions, facilitating future maintenance while providing optimal energy performance.
- Insulation installation: Primary insulation installation proceeded with special attention to health-care facility material and installation procedure requirements.
- Final installation and training: The concluding phase involved installing fabricated removable blankets and creating training materials to enable facility staff to properly remove and replace blankets during routine maintenance.
In summary, the assessment site walk was conducted in the fall of 2018, construction began in May 2021, and the project was completed by December 2023 (for all three sites).
Quality Assurance Framework and Performance Improvements
Implementation included comprehensive quality assurance measures to ensure performance met or exceeded projections. The team provided detailed “as-built” reporting, with post-installation calculations and photographic documentation of completed work.
Additionally, actual completed work scope exceeded original assessment projections, reflecting additional opportunities identified during implementation, as well as the team’s commitment to maximizing energy savings within approved budget frameworks.
The most obvious result was significant room temperature improvement throughout the facilities, with mechanical room environments becoming more comfortable for maintenance personnel, and adjacent areas showing improved climate control. These enhancements translated directly into reduced energy consumption.
Conclusion: A Replicable Framework for Health-Care Energy Efficiency
This VA hospital insulation assessment demonstrates how methodical energy conservation evaluation can deliver substantial returns while addressing unique health-care facility requirements. The project’s success reflects careful attention to technical assessment methodology, health-care-specific operational constraints, and performance frameworks, enabling guaranteed results.
Upon completion of the project, Irex provided the original calculations, along with the post-implementation calculations, as well as before and after infrared imaging that allowed the customer to see the impact of the installed insulation via the lack of heat loss through the piping. Martin noted that, in his experience, “when people walk into the room and they don’t break into a sweat like they did before, they may not notice the shiny new insulation, but they notice how they feel in the room. To us, that’s a win, because we know we helped them.”
The project established a systematic methodology balancing technical rigor with operational sensitivity, enabling similar improvements across health-care environments. Key elements include:
- Comprehensive documentation, regardless of immediate payback potential;
- A multi-technique assessment combining visual, thermal, and precision measurement approaches;
- Health-care-specific operational integration planning;
- Phased implementation strategies addressing facility and materials constraints; and
- Performance verification and training components for long-term success.
“For overall insulation performance across VA hospital facilities, every single facility I’ve been in has needs. There’s an energy conservation measure in every one of them. The ROI is compelling,” concluded Le Blanc.